15.09.2020
Preventing Bedsores
What is a bedsore?
Bedsore is a skin condition arising from the exposure to the following factors:
- Pressure over extended periods causes local ischemia, or loss of oxygen from blood flow. Cells deprived of oxygen die and extended periods of pressure lead to inflammation that can quickly develop into a bedsore.
- Friction – rubbing peels the epidermis, making the skin weaker or even damaging it. Skin irritation or damage promotes bedsore development.
- Maceration – occurs when the skin is constantly exposed to moisture, softening it and causing it to become easily infected. Agents causing macerations are:
Sweat
Urine
Wound exudation
What promotes bedsore development?
- Limited mobility – confinement, physical disability, etc.
- Injury or abrasion to the skin surface
- Improper skin care
- General health problems – e.g., malnutrition, protein deficiency, electrolyte imbalance, and cardiovascular issues.
- Atherosclerosis, diabetes, and other metabolic disorders
- Prolonged exposure to wetness which can be caused by choosing the wrong incontinence management products
- Too high of an ambient temperature, causing excessive perspiration and skin chafing
- Clothing and bedding made of artificial, irritating materials
- Internal seams in clothes, buttons, food bits or other debris in the mattress, etc.
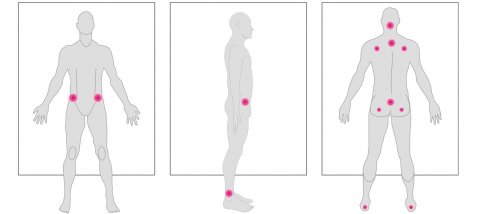
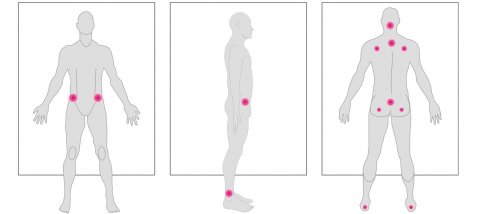
The most common places where bedsores occur
5 stages of bedsores
Bedsores are rated in 5 stages, depending on the stage of development
Stage 1 – redness that fades after eliminating pressure. There is no skin damage.
Stage 2 – redness which does not fade after relieving pressure. This stage involves surface swelling, skin erosion, and possible painful epidermis injury.
Stage 3 – deep skin damage reaching the dermis (deeper skins structure). This stage involves visible swelling and rash. The bottom of the wound may be covered with dissolving tissue (yellow mass) or red granulation.
Stage 4 – the damage reaches down to the bone. Skin necrosis occurs and dead tissue is present. The bottom of the wound may be filled with black necrotic tissue.
Stage 5 – this is the most advanced stage. Necrosis reaches down to the muscles and may lead to sepsis.
Bedsore preventive treatment
As a result, they do not develop bedsores. Bedsore development is common among people with limited mobility and can be considerably reduced by following the rules of bedsore preventive treatment.
Do not ignore the symptoms
Skin redness that is not subsiding after relieving pressure, blisters developing in the area, a damaged epidermis – these are all symptoms that should alert the carer. Constant skin observation is a crucial element of bedsore prevention.
Try to eliminate risk factors
- Body repositioning should be carried out regularly every 2–3 hours.
- Decrease pressure on the skin. If bedsores start to develop, the person you look after should not sit or lie on the body part affected.
- Remember to separate the legs with a pillow when positioning on the side.
- Get rid of rubber underpads. These tend to crease and fold, putting pressure on the skin and blocking air circulation.
- Bedding should never be wet. If the person you look after wets the bedding, it should be changed.
- Prevent injuries like scratches by clipping your loved one’s nails short and regularly filing them.
Use special preventive equipment
- Pressure reducing (anti bedsore) mattress
- Anti bedsore pillows
- Special bed underpads and mattress protectors
- Slip mats and sliding equipment used to reposition the person on the bed.
Try to engage with your loved one as much as possible
- Encourage the person under your care to stay active.
- Try to work on increasing mobility.
- Do not relieve the person you look after from every activity.
Use Skin Care products
- Delicately cleanse the skin using dedicated skin care products.
- Avoid using products that affect the skin too much. Avoid using powder with greasy products such as oil or creams.
- Remember about the intimate hygiene of the person you look after – cleanse these areas with delicate products and apply protection as needed.
- Check the skin’s condition every day. React promptly if you come across something that causes alarm.
- Activate the skin through massage.
Ensure a healthy diet for the person you look after
- Daily diet should supply the body with all necessary nutrients, vitamins, and minerals.
- The diet should include cereals, dairy products, legumes, meat, fish, fruits and vegetables.
- If bedsores start to develop, introduce a diet that is high in protein.
- Sweets, animal fat, and salt consumption should be cut down and avoided when possible.
- If bed sores develop, you need to consult a doctor immediately to plan treatment. Treatment of bedsores takes time. It can be a difficult process, however if you follow the doctor’s advice, it is possible to cure them.
Remember the sooner you start to employ proper action, the quicker and more effective the treatment will be. Bedsores – and all incontinence-related skin problems – are easier to prevent than cure.
You can find more information on proper skin care here. Get to know the practical advice for carers looking after their loved ones.